1. WHO (2017) Global Strategy and Action Plan on Ageing and Health, World Health Organisation.
2. Socialstyrelsen (2018) Vård Och Omsorg Om Äldre – Lägesrapport 2018 (Care of the Elderly – Status Report 2018), Socialstyrelsen.
3. Folkhälsomyndigheten (2018) Folkhälsans Utveckling – Årsrapport 2018 (Public Health in Sweden 2018), Folkhälsomyndigheten.
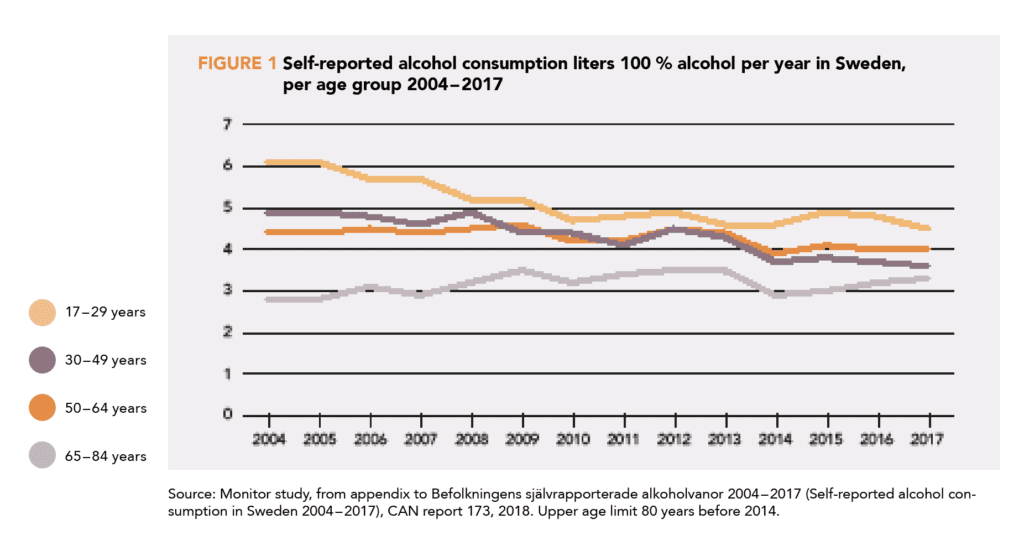
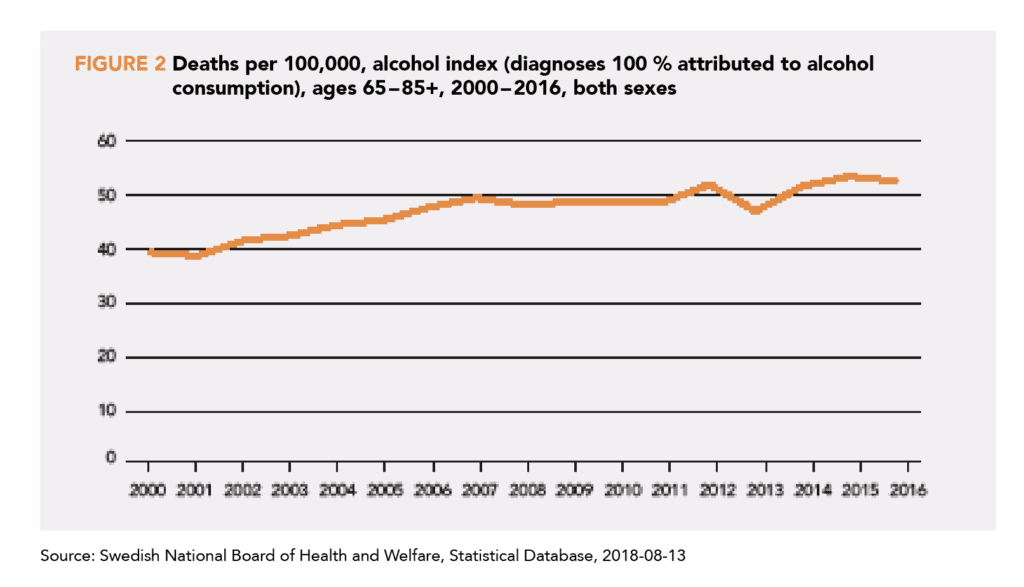
4. Socialstyrelsens statistikdatabas Available at: https://www.socialstyrelsen.se [Accessed July 4, 2018].
5. Institute for Health Metrics and Evaluation (IHME) GBD Compare Data Visualization Seattle, WA: IHME, University of Washington, 2017 Available at: http://vizhub.healthdata.org/gbd-compare [Accessed July 4, 2018].
6. Badrick E, Bobak M, Britton A, Kirschbaum C, Marmot M, Kumari M (2008) The relationship between alcohol consumption and cortisol secretion in an aging cohort. J Clin Endocrinol Metab 93, 750–7.
7. Moore AA, Whiteman EJ, Ward KT (2007) Risks of combined alcohol/medication use in older adults.
Am J Geriatr Pharmacother 5, 64–74.
8. Schneider B (2009) Substance use disorders and risk for completed suicide. Archives of suicide research 13, 303–16.
9. Kuerbis A, Sacco P (2012) The impact of retirement on the drinking patterns of older adults: a review. Addict Behav 37, 587–95.
10. WHO (2015) World Report on Ageing and Health, World Health Organization.
11. Holdsworth C, Frisher M, Mendonça M, DE Oliveiria C, Pikhart H, Shelton N (2017) Lifecourse transitions, gender and drinking in later life. Ageing Soc 37, 462–94.
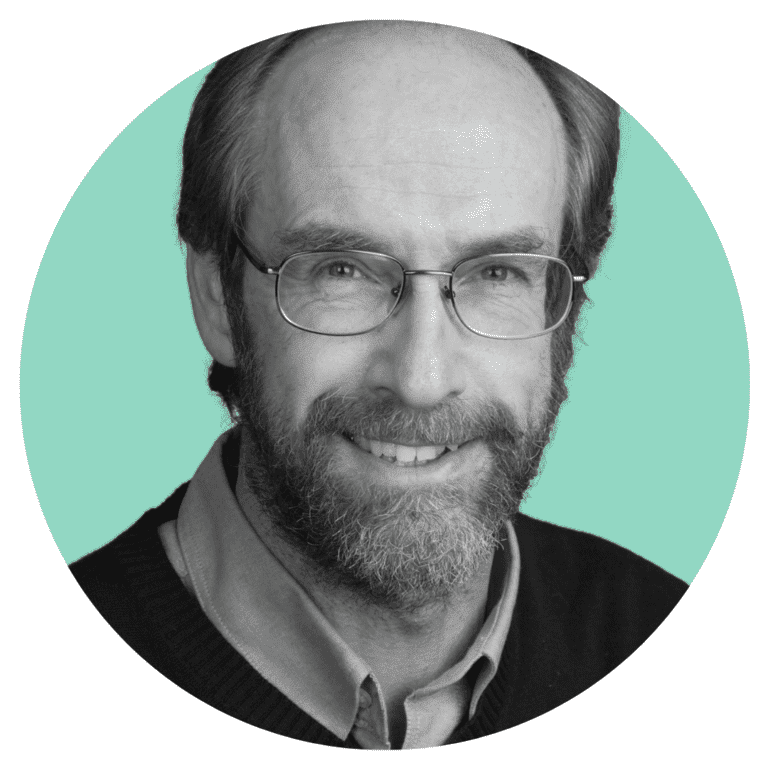
12. Guttormson U, Gröndahl M (2018) Befolkningens Självrapporterade Alkoholvanor 2004 – 2017 (Self-Reported Alcohol Consumption in Sweden 2004 – 2017), CAN.
13. Nationella folkhälsoenkäten (National Public Health Survey) Available at: https://www.folkhalsomyndigheten.se/folkhalsorapportering-statistik/statistikdatabaser-och-visualisering/nationella-folkhalsoenkaten/.
14. Waern M, Marlow T, Morin J, Ostling S, Skoog I (2014) Secular changes in at-risk drinking in Sweden: birth cohort comparisons in 75-year-old men and women 1976 –2006. Age Ageing 43, 228–34.
15. Dödsorsaker [internet] (Causes of death) Available at: https://www.socialstyrelsen.se/statistik/statistikdatabas.
16. Gordis L (2014) Epidemiology (5th Ed.), Philadelphia, PA: Elsevier/Saunders.
17. Moderate Alcohol and Cardiovascular Health Trial (MACH15) Available at: https://clinicaltrials.gov/ct2/show/NCT03169530 [Accessed August 7, 2018].
18. NIH to end funding for Moderate Alcohol and Cardiovascular Health trial Available at: https://www.nih.gov/news-events/news-releases/nih-end-funding-moderate-alcohol-cardiovascular-health-trial [Accessed August 7, 2018].
19. NIH Advisory Committee To The Director (2018) ACD Working Group for Review of the Moderate Alcohol and Cardiovascular Health Trial Available at: https://acd.od.nih.gov/documents/presentations/06152018Tabak-B.pdf.
20. Fekjaer HO (2013) Alcohol-a universal preventive agent? A critical analysis. Addiction 108, 2051–7.
21. Fillmore KM, Stockwell T, Chikritzhs T, Bostrom A, Kerr W (2007) Moderate alcohol use and reduced mortality risk: systematic error in prospective studies and new hypotheses. Ann Epidemiol 17, S16–23.
22. Caldwell TM, Rodgers B, Power C, Clark C, Stansfeld SA Drinking histories of self-identified lifetime abstainers and occasional drinkers: findings from the 1958 British Birth Cohort Study. Alcohol Alcohol 41, 650–4.
23. Ng Fat L, Shelton N (2012) Associations between self-reported illness and non-drinking in young adults. Addiction 107, 1612–20.
24. Staff J, Maggs J (2017) Alcohol and Cigarette Use From Ages 23 to 55: Links With Health and Well-Being in the Long-Term National Child Development Study. J Stud Alcohol Drugs 78, 394–403.
25. Naimi TS, Brown DW, Brewer RD, Giles WH, Mensah G, Serdula MK, Mokdad AH, Hungerford DW, et al (2005) Cardiovascular risk factors and confounders among nondrinking and moderate-drinking U.S. adults. Am J Prev Med 28, 369–73.
26. Naimi TS, Stockwell T, Zhao J, Xuan Z, Dangardt F, Saitz R, Liang W, Chikritzhs T (2017) Selection biases in observational studies affect associations between “moderate” alcohol consumption and mortality. Addiction 112, 207–14.
27. Stockwell T, Zhao J, Panwar S, Roemer A, Naimi T, Chikritzhs T (2016) Do “Moderate” Drinkers Have Reduced Mortality Risk? A Systematic Review and Meta-Analysis of Alcohol Consumption and All-Cause Mortality. J Stud Alcohol Drugs 77, 185–98.
28. Zhao J, Stockwell T, Roemer A, Naimi T, Chikritzhs T (2017) Alcohol Consumption and Mortality From Coronary Heart Disease: An Updated Meta-Analysis of Cohort Studies. J Stud Alcohol Drugs 78, 375–86.
29. Holmes MV, Dale CE, Zuccolo L, Silverwood RJ, Guo Y, Ye Z, Prieto-Merino D, Dehghan A, et al (2014) Association between alcohol and cardiovascular disease: Mendelian randomisation analysis based on individual participant data. BMJ 349, g4164.
30. GBD 2016 Alcohol Collaborators (2018) Alcohol use and burden for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 392, 1015–35.
31. Bagnardi V, Zambon A, Quatto P, Corrao G (2004) Flexible meta-regression functions for modeling aggregate dose-response data, with an application to alcohol and mortality. Am J Epidemiol 159, 1077–86.
32. Collins D, Lapsley H (2008) The Costs of Tobacco, Alcohol and Illicit Drug Abuse to Australian Society in 2004/05., Canberra: Australian Department of Health and Ageing.
33. Laslett A-M, Catalano P, Chikritzhs Y, Dale C, Doran C, Ferris J, Jainullabudeen T, Livingston M, et al (2010) The Range and Magnitude of Alcohol’s Harm to Others., Fitzroy, Victoria: AER Centre for Alcohol Policy Research, Turning Point Alcohol and Drug Centre, Eastern Health.
34. Chikritzhs TN, Naimi TS, Stockwell TR, Liang W (2015) Mendelian randomisation meta-analysis sheds doubt on protective associations between “moderate” alcohol consumption and coronary heart disease.
Evid Based Med 20, 38.
35. Colpani V, Baena CP, Jaspers L, van Dijk GM, Farajzadegan Z, Dhana K, Tielemans MJ, Voortman T, et al (2018) Lifestyle factors, cardiovascular disease and all-cause mortality in middle-aged and elderly women: a systematic review and meta-analysis.
Eur J Epidemiol. doi:10.1007/s10654-018-0374-z.
36. Di Castelnuovo A, Costanzo S, Bagnardi V, Donati MB, Iacoviello L, de Gaetano G (2006) Alcohol dosing and total mortality in men and women: an updated meta-analysis of 34 prospective studies. Arch Intern Med 166, 2437–45.
37. Ferrari P, Licaj I, Muller DC, Kragh Andersen P, Johansson M, Boeing H, Weiderpass E, Dossus L, et al (2014) Lifetime alcohol use and overall and cause-specific mortality in the European Prospective Investigation into Cancer and nutrition (EPIC) study. BMJ Open 4, e005245.
38. Kunzmann AT, Coleman HG, Huang W-Y, Berndt SI (2018) The association of lifetime alcohol use with mortality and cancer risk in older adults: A cohort study. PLoS medicine 15, e1002585.
39. Wood AM, Kaptoge S, Butterworth AS, Willeit P, Warnakula S, Bolton T, Paige E, Paul DS, et al (2018) Risk thresholds for alcohol consumption: combined analysis of individual-participant data for 599 912 current drinkers in 83 prospective studies. Lancet 391, 1513–23.
40. Almeida OP, McCaul K, Hankey GJ, Yeap BB, Golledge J, Flicker L (2017) Excessive alcohol consumption increases mortality in later life: a genetic analysis of the health in men cohort study. Addict Biol 22, 570–8.
41. Knott CS, Coombs N, Stamatakis E, Biddulph JP (2015) All cause mortality and the case for age specific alcohol consumption guidelines: pooled analyses of up to 10 population based cohorts. BMJ 350, h384.
42. Au Yeung SL, Jiang C, Cheng KK, Cowling BJ, Liu B, Zhang W, Lam TH, Leung GM, Schooling CM (2013) Moderate alcohol use and cardiovascular disease from Mendelian randomization. PLoS ONE 8, e68054.
43. Yun KE, Chang Y, Yun S-C, Davey Smith G, Ryu S, Cho S-I, Chung EC, Shin H, Khang Y-H (2017) Alcohol and coronary artery calcification: an investigation using alcohol flushing as an instrumental variable. Int J Epidemiol 46, 950–62.
44. De Lorgeril M, Salen P, Martin JL, Monjaud I, Delaye J, Mamelle N (1999) Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: final report of the Lyon Diet Heart Study. Circulation 99, 779–85.
45. Estruch R, Ros E, Salas-Salvadó J, Covas M-I, Corella D, Arós F, Gómez-Gracia E, Ruiz-Gutiérrez V, et al (2013) Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med 368, 1279–90.
46. Patra J, Taylor B, Irving H, Roerecke M, Baliunas D, Mohapatra S, Rehm J (2010) Alcohol consumption and the risk of morbidity and mortality for different stroke types-a systematic review and meta-analysis. BMC Public Health 10, 258.
47. Rehm J, Shield KD, Roerecke M, Gmel G (2016) Modelling the impact of alcohol consumption on cardiovascular disease mortality for comparative risk assessments: an overview. BMC Public Health 16, 363.
48. Taylor B, Irving HM, Baliunas D, Roerecke M, Patra J, Mohapatra S, Rehm J (2009) Alcohol and hypertension: gender differences in dose-response relationships determined through systematic review and meta-analysis. Addiction 104, 1981–90.
49. Roerecke M, Kaczorowski J, Tobe SW, Gmel G, Hasan OSM, Rehm J (2017) The effect of a reduction in alcohol consumption on blood pressure: a systematic review and meta-analysis. Lancet Public Health 2, e108–e120.
50. Chen L, Smith GD, Harbord RM, Lewis SJ (2008) Alcohol intake and blood pressure: a systematic review implementing a Mendelian randomization approach. PLoS Med 5, e52.
51. Baliunas DO, Taylor BJ, Irving H, Roerecke M, Patra J, Mohapatra S, Rehm J (2009) Alcohol as a risk factor for type 2 diabetes: A systematic review and meta-analysis. Diabetes Care 32, 2123–32.
52. Kerr WC, Ye Y (2010) Relationship of life-course drinking patterns to diabetes, heart problems, and hypertension among those 40 and older in the 2005 U.S. National Alcohol Survey. J Stud Alcohol Drugs 71, 515–25.
53. Knott C, Bell S, Britton A (2015) Alcohol Consumption and the Risk of Type 2 Diabetes: A Systematic Review and Dose-Response Meta-analysis of More Than 1.9 Million Individuals From 38 Observational Studies. Diabetes Care 38, 1804–12.
54. Cho Y, Shin S-Y, Won S, Relton CL, Davey Smith G, Shin M-J (2015) Alcohol intake and cardiovascular risk factors: A Mendelian randomisation study. Sci Rep 5, 18422.
55. Lawlor DA, Nordestgaard BG, Benn M, Zuccolo L, Tybjaerg-Hansen A, Davey Smith G (2013) Exploring causal associations between alcohol and coronary heart disease risk factors: findings from a Mendelian randomization study in the Copenhagen General Population Study. Eur Heart J 34, 2519–28.
56. Hirst J, Aronson J, Feakins B, Ma C, Farmer A, Stevens R (2017) Short-and medium-term effects of light to moderate alcohol intake on glycaemic control in diabetes mellitus: a systematic review and meta-analysis of randomized trials. Diabetic Medicine 34, 604–11.
57. Briel M, Ferreira-Gonzalez I, You JJ, Karanicolas PJ, Akl EA, Wu P, Blechacz B, Bassler D, et al (2009) Association between change in high density lipoprotein cholesterol and cardiovascular disease morbidity and mortality: systematic review and meta-regression analysis. BMJ 338, b92.
58. Schwartz GG, Olsson AG, Abt M, Ballantyne CM, Barter PJ, Brumm J, Chaitman BR, Holme IM, et al (2012) Effects of dalcetrapib in patients with a recent acute coronary syndrome. N Engl J Med 367, 2089–99.
59. Voight BF, Peloso GM, Orho-Melander M, Frikke-Schmidt R, Barbalic M, Jensen MK, Hindy G, Hólm H, et al (2012) Plasma HDL cholesterol and risk of myocardial infarction: a mendelian randomisation study. Lancet 380, 572–80.
60. Brien SE, Ronksley PE, Turner BJ, Mukamal KJ, Ghali WA (2011) Effect of alcohol consumption on biological markers associated with risk of coronary heart disease: systematic review and meta-analysis of interventional studies. BMJ 342, d636.
61. Berger NA, Savvides P, Koroukian SM, Kahana EF, Deimling GT, Rose JH, Bowman KF, Miller RH (2006) Cancer in the elderly. Trans Am Clin Climatol Assoc 117, 147–55; discussion 155–6.
62. IARC (2010) Alcohol Consumption and Ethyl Carbamate. IARC Monographs on the Evaluation
of Carcinogenic Risks to Humans. (Vol. 96), Lyon, France: IARC.
63. World Cancer Research Fund International/American Institute for Cancer Research (2016) Continuous Update Project Report: Diet, Nutrition, Physical Activity and Stomach Cancer. London: WCRF.
64. Bagnardi V, Rota M, Botteri E, Tramacere I, Islami F, Fedirko V, Scotti L, Jenab M, et al (2015) Alcohol consumption and site-specific cancer risk: a comprehensive dose-response meta-analysis.
Br J Cancer 112, 580–93.
65. Michael J, Howard LE, Markt SC, De Hoedt A, Bailey C, Mucci LA, Freedland SJ, Allott EH (2018) Early-Life Alcohol Intake and High-Grade Prostate Cancer: Results from an Equal-Access, Racially Diverse Biopsy Cohort. Cancer Prev Res (Phila) 11, 621–8.
66. Zhao J, Stockwell T, Roemer A, Chikritzhs T (2016) Is alcohol consumption a risk factor for prostate cancer? A systematic review and meta-analysis. BMC Cancer 16, 845.
67. Andreasson S, Chikritzhs T, Dangardt F, Holder H, Naimi T, Stockwell T (2016) Alcohol and Society: Alcohol and Cancer, Stockholm: Swedish Society of Medicine & IOGT-NTO.
68. Sherk A, Stockwell T, Rehm J, Dorocicz J, Shield KD (2017) The International Model of Alcohol Harms and Policies (InterMAHP): A Comprehensive Guide to the Estimation of Alcohol-Attributable Morbidity and Mortality., Canadian Institute for Substance Use Research, University of Victoria, British Columbia, Canada. Available at: www.intermahp.cisur.ca.
69. Schwarzinger M, Pollock BG, Hasan OSM, Dufouil C, Rehm J (2018) Contribution of alcohol use disorders to the burden of dementia in France 2008-13: a nationwide retrospective cohort study. Lancet Public Health 3, e124–e132.
70. Winblad B, Amouyel P, Andrieu S, Ballard C, Brayne C, Brodaty H, Cedazo-Minguez A, Dubois B, et al (2016) Defeating Alzheimer’s disease and other dementias: a priority for European science and society. Lancet Neurol 15, 455–532.
71. Downer B, Zanjani F, Fardo DW (2014) The relationship between midlife and late life alcohol consumption, APOE e4 and the decline in learning and memory among older adults. Alcohol Alcohol 49, 17–22.
72. Verbaten MN (2009) Chronic effects of low to moderate alcohol consumption on structural and functional properties of the brain: beneficial or not? Hum Psychopharmacol 24, 199–205.
73. Almeida OP, Hankey GJ, Yeap BB, Golledge J, Flicker L (2014) Alcohol consumption and cognitive impairment in older men: a mendelian randomization study. Neurology 82, 1038–44.
74. Kroenke CD, Rohlfing T, Park B, Sullivan EV, Pfefferbaum A, Grant KA (2014) Monkeys that voluntarily and chronically drink alcohol damage their brains: a longitudinal MRI study. Neuropsychopharmacology 39, 823–30.
75. WHO (2017) Global Action Plan on the Public Health Response to Dementia 2017 – 2025. Geneva: World Health Organization; 2017.
76. Martínez-Lapiscina EH, Clavero P, Toledo E, Estruch R, Salas-Salvadó J, San Julián B, Sanchez-Tainta A, Ros E, et al (2013) Mediterranean diet improves cognition: the PREDIMED-NAVARRA randomised trial. J Neurol Neurosurg Psychiatry 84, 1318–25.
77. Sabia S, Fayosse A, Dumurgier J, Dugravot A, Akbaraly T, Britton A, Kivimäki M, Singh-Manoux A (2018) Alcohol consumption and risk of dementia: 23 year follow-up of Whitehall II cohort study. BMJ 362, k2927.
78. Topiwala A, Ebmeier KP (2018) Effects of drinking on late-life brain and cognition. Evid Based Ment Health 21, 12–5.
79. Hassing LB (2018) Light Alcohol Consumption Does Not Protect Cognitive Function: A Longitudinal Prospective Study. Front Aging Neurosci 10, 81.
80. Cherpitel CJ (2007) Alcohol and injuries: a review of international emergency room studies since 1995. Drug Alcohol Rev 26, 201–14.
81. Taylor B, Irving HM, Kanteres F, Room R, Borges G, Cherpitel C, Greenfield T, Rehm J (2010) The more you drink, the harder you fall: a systematic review and meta-analysis of how acute alcohol consumption and injury or collision risk increase together. Drug Alcohol Depend 110, 108–16.
82. Zeisser C, Stockwell TR, Chikritzhs T, Cherpitel C, Ye Y, Gardner C (2013) A systematic review and meta-analysis of alcohol consumption and injury risk as a function of study design and recall period. Alcohol Clin Exp Res 37 Suppl 1, E1–8.
83. Dionyssiotis Y (2012) Analyzing the problem of falls among older people. Int J Gen Med 5, 805–13.
84. Fell JC, Scherer M (2017) Estimation of the Potential Effectiveness of Lowering the Blood Alcohol Concentration (BAC) Limit for Driving from 0.08 to 0.05 Grams per Deciliter in the United States. Alcohol Clin Exp Res 41, 2128–39.
85. Taylor B, Rehm J (2012) The relationship between alcohol consumption and fatal motor vehicle injury: high risk at low alcohol levels. Alcohol Clin Exp Res 36, 1827–34.
86. Dadgar I, Norström T (2017) Short-term and long-term effects of GDP on traffic deaths in 18 OECD countries, 1960-2011. J Epidemiol Community Health 71, 146–53.
87. Martin TL, Solbeck PAM, Mayers DJ, Langille RM, Buczek Y, Pelletier MR (2013) A review of alcohol-impaired driving: the role of blood alcohol concentration and complexity of the driving task.
J Forensic Sci 58, 1238–50.
88. Santos AMR dos, Rodrigues RAP, Diniz MA (2015) Trauma in the elderly caused by traffic accident: integrative review. Rev Esc Enferm USP 49, 162–72.
89. IIHS (2016) Fatality facts 2015, Older people. Available at: http://www.iihs.org/iihs/topics/t/older-drivers/fatalityfacts/older-people/2015 [Accessed August 14, 2018].
90. Sklar AL, Boissoneault J, Fillmore MT, Nixon SJ (2014) Interactions between age and moderate alcohol effects on simulated driving performance. Psychopharmacology (Berl) 231, 557–66.
91. Scheetz LJ (2015) One for the Road: A Comparison of Drinking and Driving Behavior Among Younger and Older Adults Involved in Fatal Crashes. J Trauma Nurs 22, 187–93.
92. Ridolfo B, Stevenson C (2001) The Quantification of Drug-Caused Mortality and Morbidity in Australia, 1998, Australian Institute of Health and Welfare.
93. Wu HZ, Barry LC, Duan Y, Bohannon RW, Covault JM, Grady JJ (2017) Acute Effects of Moderate Alcohol Consumption on Postural Stability in Older Adults. Percept Mot Skills 124, 912–31.
94. Li Y, Jensen GA (2012) Effects of drinking on hospital stays and emergency room visits among older adults. J Aging Health 24, 67–91.
95. Tait RJ, French DJ, Burns RA, Byles JE, Anstey KJ (2013) Alcohol, hospital admissions, and falls in older adults: a longitudinal evaluation. Int Psychogeriatr 25, 901–12.
96. Berg KM, Kunins HV, Jackson JL, Nahvi S, Chaudhry A, Harris KA, Malik R, Arnsten JH (2008) Association between alcohol consumption and both osteoporotic fracture and bone density. Am J Med 121, 406–18.
97. Drake MT, Murad MH, Mauck KF, Lane MA, Undavalli C, Elraiyah T, Stuart LM, Prasad C, et al (2012) Clinical review. Risk factors for low bone mass-related fractures in men: a systematic review and meta-analysis. J Clin Endocrinol Metab 97, 1861–70.
98. Papaioannou A, Kennedy CC, Cranney A, Hawker G, Brown JP, Kaiser SM, Leslie WD, O’Brien CJM, et al (2009) Risk factors for low BMD in healthy men age 50 years or older: a systematic review. Osteoporos Int 20, 507–18.
99. Waugh EJ, Lam M-A, Hawker GA, McGowan J, Papaioannou A, Cheung AM, Hodsman AB, Leslie WD, et al (2009) Risk factors for low bone mass in healthy 40-60 year old women: a systematic review of the literature. Osteoporos Int 20, 1–21.
100. Kubo JT, Stefanick ML, Robbins J, Wactawski-Wende J, Cullen MR, Freiberg M, Desai M (2013) Preference for wine is associated with lower hip fracture incidence in post-menopausal women. BMC Womens Health 13, 36.
101. Ortolá R, García-Esquinas E, Galán I, Guallar-Castillón P, López-García E, Banegas JR, Rodríguez-Artalejo F (2017) Patterns of alcohol consumption and risk of falls in older adults: a prospective cohort study. Osteoporos Int 28, 3143–52.
102. Yon Y, Mikton C, Gassoumis Z, Wilber K (2017) Elder abuse prevalence in community settings: a systematic review and meta-analysis. Lancet Glob Health 5, e147–e156.
103. Pillemer K, Burnes D, Riffin C, Lachs MS (2016) Elder Abuse: Global Situation, Risk Factors, and Prevention Strategies. Gerontologist 56 Suppl 2, S194–205.
104. Ahnlund P, Andersson T, Snellman F, Sundström M, Heimer G (2017) Prevalence and Correlates of Sexual, Physical, and Psychological Violence Against Women and Men of 60 to 74 Years in Sweden. J Interpers Violence, 886260517696874.
105. Warmling D, Lindner SR, Coelho EBS (2017) Intimate partner violence prevalence in the elderly and associated factors: systematic review. Cien Saude Colet 22, 3111–25.
106. Murphy K, Waa S, Jaffer H, Sauter A, Chan A (2013) A literature review of findings in physical elder abuse. Can Assoc Radiol J 64, 10–4.
107. Caputo F, Vignoli T, Leggio L, Addolorato G, Zoli G, Bernardi M (2012) Alcohol use disorders in the elderly: a brief overview from epidemiology to treatment options. Exp Gerontol 47, 411–6.
108. Borges G, Loera CR (2010) Alcohol and drug use in suicidal behaviour. Current Opinion in Psychiatry 23, 195–204.
109. Blow FC, Brockmann LM, Barry KL (2004) Role of alcohol in late-life suicide. Alcohol Clin Exp Res 28, 48S–56S.
110. Hilton ME (1987) Demographic characteristics and the frequency of heavy drinking as predictors of self-reported drinking problems. Br J Addict 82, 913–25.
111. Midanik LT, Clark WB (1995) Drinking-related problems in the United States: description and trends, 1984-1990. J Stud Alcohol 56, 395–402.
112. Mäkelä K, Mustonen H (2000) Relationships of drinking behaviour, gender and age with reported negative and positive experiences related to drinking. Addiction 95, 727–36.
113. Jacobs LG, Berman A (2003) Respiratory disease in the elderly. Clinics in Geriatric Medicine 19, xi – xii .
114. Cunha BA (2001) Pneumonia in the elderly. Clinical Microbiology and Infection 7, 581 – 588.
115. Samokhvalov AV, Irving HM, Rehm J (2010) Alcohol consumption as a risk factor for pneumonia: a systematic review and meta-analysis. Epidemiol Infect 138, 1789–95.
116. Kuo C-F, Grainge MJ, Zhang W, Doherty M (2015) Global epidemiology of gout: prevalence, incidence and risk factors. Nat Rev Rheumatol 11, 649–62.
117. Zhu Y, Pandya BJ, Choi HK (2011) Prevalence of gout and hyperuricemia in the US general population: the National Health and Nutrition Examination Survey 2007-2008. Arthritis Rheum 63, 3136–41.
118. Singh JA, Reddy SG, Kundukulam J (2011) Risk factors for gout and prevention: a systematic review of the literature. Curr Opin Rheumatol 23, 192–202.
119. Wang M, Jiang X, Wu W, Zhang D (2013) A meta-analysis of alcohol consumption and the risk of gout. Clin Rheumatol 32, 1641–8.
120. Roddy E, Zhang W, Doherty M (2007) Are joints affected by gout also affected by osteoarthritis?
Ann Rheum Dis 66, 1374–7.
121. Kc R, Voigt R, Li X, Forsyth CB, Ellman MB, Summa KC, Turek FW, Keshavarzian A, et al (2015) Induction of Osteoarthritis-like Pathologic Changes by Chronic Alcohol Consumption in an Experimental Mouse Model. Arthritis & rheumatology (Hoboken, NJ) 67, 1678–80.
122. Batista P, Pereira A (2016) Quality of Life in Patients with Neurodegenerative Diseases.
123. Ishihara LS, Cheesbrough A, Brayne C, Schrag A (2007) Estimated life expectancy of Parkinson’s patients compared with the UK population. J Neurol Neurosurg Psychiatr 78, 1304–9.
124. Bettiol SS, Rose TC, Hughes CJ, Smith LA (2015) Alcohol Consumption and Parkinson’s Disease Risk: A Review of Recent Findings. J Parkinsons Dis 5, 425–42.
125. Dufour MC, Archer L, Gordis E (1992) Alcohol and the elderly. Clin Geriatr Med 8, 127–41.
126. Ebrahim IO, Shapiro CM, Williams AJ, Fenwick PB (2013) Alcohol and sleep I: effects on normal sleep. Alcohol Clin Exp Res 37, 539–49.
127. Roehrs T, Roth T (2001) Sleep, sleepiness, sleep disorders and alcohol use and abuse. Sleep Med Rev 5, 287–97.
128. Stein MD, Friedmann PD (2005) Disturbed sleep and its relationship to alcohol use. Subst Abus 26, 1–13.
129. Raninen J, Härkönen J, Landberg J (2016) Long-term effects of changes in Swedish alcohol policy: can alcohol policies effective during adolescence impact consumption during adulthood? Addiction 111, 1021–6.
130. Babor TF, Babor T, Caetano R, Casswell S, Edwards G, Giesbrecht N (2010) Alcohol: No Ordinary Commodity: Research and Public Policy, Oxford University Press.
131. Nelson TF, Xuan Z, Babor TF, Brewer RD, Chaloupka FJ, Gruenewald PJ, Holder H, Klitzner M, et al (2013) Efficacy and the strength of evidence of U.S. alcohol control policies. Am J Prev Med 45, 19–28.
132. Holmes J, Meng Y, Meier PS, Brennan A, Angus C, Campbell-Burton A, Guo Y, Hill-McManus D, Purshouse RC (2014) Effects of minimum unit pricing for alcohol on different income and socioeconomic groups: a modelling study. Lancet 383, 1655–64.
133. Zhao J, Stockwell T (2017) The impacts of minimum alcohol pricing on alcohol attributable morbidity in regions of British Colombia, Canada with low, medium and high mean family income. Addiction 112, 1942–51.
134. Brady JE, Baker SP, Dimaggio C, McCarthy ML, Rebok GW, Li G (2009) Effectiveness of mandatory alcohol testing programs in reducing alcohol involvement in fatal motor carrier crashes. Am J Epidemiol 170, 775–82.
135. US Dietary Guidelines 2015-2020, appendix 9, Alcohol (2015) Available at: https://health.gov/dietaryguidelines/2015/guidelines/appendix-9/ [Accessed August 15, 2018].
136. National Health and Medical Research Council (2009) Australian Guidelines to Reduce Health Risks from Drinking Alcohol., Canberra: Commonwealth of Australia.
137. Scafato E, Galluzzo L, Ghirini S, Gandin C, Martire S Low risk drinking guidelines in Europe: overview of RARHA survey results. Available at: http://www.rarha.eu/Resources/Guidelines/Documents/Overview%20WP5_T1%20LowRiskDrinkingGuidelines_FINAL.pdf [Accessed August 14, 2018].
138. Butt P, Beirness D, Cesa F, Gliksman L, Paradis C, Stockwell T (2011) Alcohol and Health in Canada: A Summary of Evidence and Guidelines for Low-Risk Drinking, Canadian Centre on Sustance Abuse.